What’s Acute Respiratory Distress Syndrome?

- 1.
- 2. Frequent symptoms of ARDS – acute respiratory distress syndrome
- 3. What conditions within the lungs make this syndrome so hard to treat?
- 4. Timely efforts to properly diagnose ARDS and other lung conditions are critical
- 5. Besides pneumonia, sepsis and TBIs – here are other direct causes of some ARDS cases
- 6. Current treatments for ARDS
- 7. Prognosis for many ARDS patients
- 8. Precise aspects of the internal damage harming patients while ARDS afflicts them
After suffering a traumatic brain injury, accident survivors can develop a wide array of critical medical problems, including major breathing difficulties. Immediate medical care must be obtained so the affected person can keep breathing, and the brain can avoid losing crucial oxygen. Too many lives are lost as emergency workers try to determine whether a patient is coping with ARDS, acute respiratory distress syndrome, or another major breathing disorder.
The Yale medical website describes ARDs as a “potentially fatal” lung condition that can lead to numerous organs failing to receive adequate oxygen required for their proper functioning. Each year, about 190,000 Americans are diagnosed with ARDS. Fortunately, many patients can heal or greatly improve after a mechanical ventilator provides them with supplemental oxygen.
Further information is shared below concerning this lung condition that affects a significant number of traumatic brain injury (TBI) patients. Facts concerning how this condition develops and why it’s so difficult to treat are provided – along with ARDS symptoms and common diagnostic testing. Current treatments are also noted.
Frequent symptoms of ARDS – acute respiratory distress syndrome
This serious lung condition can develop as quickly as a few hours after a head injury, infection, or other malady – or it can take up to an entire week to fully appear. Here are some of the most frequently seen symptoms.
- Severe shortness of breath
- Very rapid or labored breathing
- Low blood pressure
- Extreme fatigue and a feeling of confusion
What conditions within the lungs make this syndrome so hard to treat?
Our lungs consist of roughly 500 million small air sacs (alveoli) that are surrounded by a vast number of capillaries or blood vessels. While direct physical injuries to the lungs can quickly cause damage, so can more indirect ones such as traumatic brain injuries, infections, and other negative events.
Contact our team at (212) 222-1111 for your free case evaluation.
Sadly, pneumonia and sepsis cause about 40 to 60 percent of ARDS cases. As most people know, pneumonia tends to inflame air sacs, often filling them with infectious pus and various fluids. Sepsis, a condition that involves the body’s infection-fighting process turning in on itself, can cause multiple organs to start malfunctioning, directly threatening a patient’s life. Once patients must fight ARDS as well as pneumonia or sepsis, they can soon lose their lives.
While ARDS patients are being treated in hospitals, their conditions can quickly worsen if they must undergo surgery, receive a massive blood transfusion, or develop COVID-19 (or one of its derivatives).
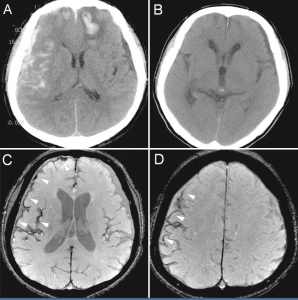
Timely efforts to properly diagnose ARDS and other lung conditions are critical
Unfortunately, there is no single test that can readily help doctors determine that a patient has ARDS. However, the following simple steps and procedures can provide strong clues – along with the multiple diagnostic tests listed below. Great care is required to isolate the presence of this specific illness.
- A doctor will use a stethoscope to listen carefully to the patient’s lungs. She is checking for what are called “crackling sounds” — common to ARDS – due to the lungs being filled with fluids.
- The patient’s heart rate and blood pressure must be measured.
- A pulse oximeter test should be performed This lets the medical staff document a possibly low blood oxygen level. Children and adults of all ages tolerate this test well since it just involves clipping a very small electronic device onto someone’s ear lobe or fingertip.
- A blood draw should be performed. This helps rules out some diseases, while signaling the possible presence of others. Problems with organ functioning levels and signs of infection often appear in blood tests results.
- One or more X-rays may be needed
- A CT (computed tomography) test. X-rays and CT scans can provide images of the fluid build-up in the lungs.
- An electrocardiogram (ultrasound image) of the patient’s heart may be ordered. This can help doctors rule out heart conditions that may mimic ARDS symptoms.
- A bronchoscopy may be required. This test involves placing a small tube (containing a camera) into the patient’s lung tissues for a closer look and evaluation.
Besides pneumonia, sepsis and TBIs – here are other direct causes of some ARDS cases
- Inhaling toxic substances
- Chest trauma that leads to serious bruising
- Almost drowning
- The development of a fat embolism (within the pulmonary system)
- Aspiration (breathing in stomach contents)
- Complications of a lung transplant
- Viral infections that develop within the lungs – such as those related to SARS-COV-2. the coronavirus that can lead to a COVID-19 infection
Other indirect causes or events can also lead to ARDS developing in someone’s lungs.
- A drug overdose
- Severe trauma to parts of the body besides the lungs, including multiple bone fractures or burns
- Pancreatitis
Current treatments for ARDS
Patients require immediate attempts to raise their blood oxygen levels.
- Ventilation through oxygen treatments. While being hospitalized in intensive care units, most patients are placed on some form of mechanical ventilation. Although it’s useful to have these machines take over breathing functions – it can be difficult to wean some patients off them.
- Symptom treatment using medications. Diuretics are often prescribed since they help the
body dispose of excess fluids in the lungs and elsewhere. Pain medications are also requested or needed by many ARDS patients.
- Aggressive treatment of all underlying causes of ARDS. This could include specialized treatments to rid the body of inhaled toxins – or appropriately addressing burn injuries.
- Placing the patients on their bellies at least part of the time. This periodic approach to the treatment process has been useful in addressing COVID-19 complications. This simply allows other parts of the lungs to be exercised or used during ventilator or other treatments.
When one or more of the treatments above fail to help patients, some of them may be placed on ECMO (extracorporeal membrane oxygenation) therapy. This comprehensive approach can take over not just lung breathing capabilities – but also heart functions. Yet weaning a patient off ECMO can be rather difficult in many instances.
Prognosis for many ARDS patients
Given the severity of ARDS, many patients (25 to 40 % of them) may die. However, rather aggressive treatment options are proving helpful for many. For example, Yale has developed a STEPS-ICU program that is designed to have both physical and occupational therapists begin helping patients recover from their conditions while still in the ICU as promising signs of improvement appear.
Contact our team at (212) 222-1111 for your free case evaluation.
Literature available on the Yale Medicine website also addresses how patients are treated who develop (or already have such conditions) as COPD (chronic obstructive pulmonary disease), COVID-19, Long COVID, and the adult form of cystic fibrosis.
As might be guessed, failing to treat the underlying causes of ARDS – if not directly due to a traumatic brain injury – can play a very direct role in causing the early death of a patient.
Precise aspects of the internal damage harming patients while ARDS afflicts them
Once the ARDS lung damage has begun, inflamed cytokines (proteins) go to work, helping to control the activity and growth of other immune system cells and bloods cells. The entire process is very complex – yet readers with advanced medical knowledge can read further about it in this UpToDate article under the “Injury” heading and others. Even a brief or cursory review of this material makes it clear that patients’ bodies are often quickly overwhelmed by ARDS.
Complications often suffered by some (but not all) ARDS patients
- A collapsed lung or pneumothorax. This can still occur even with the use of a ventilator since these machines can cause gas to pass through a hole in the outside portion of a lung, causing it to collapse.
- Blood clots can form. A patient’s lack of activity can easily lead to the formation of blood clots, especially in the legs. The greatest danger is that one of these clots will break off and travel into one or both of the lungs where it can block blood flow as a pulmonary embolism.
- Infections can develop due to treatment. Since a patient on a ventilator requires a tube to be inserted into the windpipe, germs tend to form in that area and can injure the lungs.
- Pulmonary fibrosis or scarring. ARDS can cause a thickening or scarring in the lungs between the air sacs. This causes the lungs to stiffen, making it harder for oxygen to travel from the lungs’ air sacs into the bloodstream.
While many more ARDS patients are managing to survive today, they are likely to carry residual breathing problems with them during their later lives. These may become most noticeable as they try to take part in competitive or extreme sports activities that require strong lung functioning.
If you have suffered a traumatic brain injury after an accident caused by someone else’s negligence, you need to contact our New York City traumatic brain injury law firm. We will carefully investigate all the facts of your case, review all your medical records, and then fight hard to win the maximum compensation available to you. We want every client to fully recover for all lost wages, pain and suffering, medical expenses, and other losses.
Contact our team at (212) 222-1111 for your free case evaluation.